Dysentery Co
Substance Background
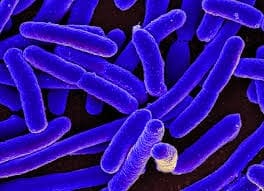
Dysentery Co is a bowel nosode prepared from a culture containing dysentery-type bacilli (historically grouped under Bacillus dysenteriae, now largely classified among Shigella spp.) and associated non-lactose-fermenting intestinal organisms. It is one of the Bach bowel nosodes, originally isolated from the stools of chronically ill patients whose symptoms shared a striking relation with the flora pattern. These organisms were attenuated and first used as autogenous vaccines; Bach later potentised them according to homeopathic principles, forming the Dysentery Co nosode for clinical use. In Paterson’s later synthesis, Dysentery Co was recognised as representing a distinct “autonomic tension” group of bowel flora, with characteristic mental and gastrointestinal symptoms.
Proving Information
Dysentery Co has no formal Hahnemannian proving; its pathogenesis is derived from long clinical observation and bacteriological correlation in the work of Bach and Paterson. Bach first observed that when potentised stool cultures containing dysentery-type bacilli were given to patients with chronic gastrointestinal and nervous complaints, a reproducible complex of mental and physical changes arose and then resolved. Paterson later refined the picture, stressing “nervous tension of an anticipatory type” and selective action on the pylorus and upper small intestine, and on the autonomic innervation of heart and mucous membranes. Contemporary authors confirm that Dysentery Co shows a consistent mental picture of anxiety, anticipatory fear and “bloody terror,” with diarrhoea or cramps triggered by emotional stress. Thus Dysentery Co is fundamentally a [Clinical] and [Toxicology]-inferred nosode rather than a classical proving remedy.
Remedy Essence
The essence of Dysentery Co is anticipatory autonomic tension expressed through the bowel and heart. It is the picture of the person whose nervous system “lives in tomorrow,” reacting to imagined events as if they were present dangers. The gut becomes the primary stage: pyloric spasm, churning, colitis and diarrhoea are the physical language of their fears.
This is not the paralysing fear of Gelsemium, where legs tremble and mind goes blank. Nor is it the impulsive, excitable anxiety of Argentum nitricum, who rushes towards events with reckless haste. Dysentery Co’s anxiety is more contained and internalised—hyper-vigilant, scanning for threats, fearful of criticism and failure, with a strong need for predictability and control. The person may appear composed, but within they are rehearsing every possible failure, and the colon faithfully broadcasts this rehearsal as cramps, mucus and loose stools.
Historically, the nosode emerges from the dysentery bacillus—symbol of a profound disturbance of the intestinal mucosa. In chronic Dysentery Co states, overt infection has passed, but the memory of dysentery lives on as hypersensitivity of the colon and the enteric nervous system. Emotional stress becomes a surrogate pathogen; anticipation alone can trigger “mini-dysenteric” episodes with urgency and gripping pains. This dramatises the gut–brain axis long before modern science described it.
At the miasmatic level, the pattern is largely psoric functional disturbance: symptoms are dramatic yet reversible; tissue damage is limited; and the organism is quick to react but equally quick to settle once safety is perceived. Sycosis contributes chronicity and recurrence—repeated bouts of IBS-type behaviour, patterning the autonomic system through habit. Tubercular colouring appears in thin, nervous students and professionals, lowered resistance after infections and alternating bowel–airway issues.
The central polarity of Dysentery Co is between control and loss of control. The patient craves control over events and over their bodily functions, yet fears losing that control in public—soiling themselves, collapsing, “going blank” under scrutiny. Every exam, speech or journey becomes a potential humiliation. Hypersensitivity to criticism feeds this polarity; a single negative comment may be ruminated on for months, fuelling future anticipatory storms.
Clinically, we see Dysentery Co in:
- Children and adolescents with school or exam anxiety, loose stools before tests, abdominal pain on school mornings, fear of teachers’ criticism and dreams of failing.
- Adults with IBS linked to work stress, public speaking, travel or medical procedures, whose colon reacts instantly to imagined scenarios, despite normal investigations.
- Post-dysenteric or post-gastro-enteritis patients who “never got their bowels back,” now living with post-infective IBS and increased anxiety about leaving safe toilet access.
Dysentery Co occupies a unique niche among bowel nosodes. Morgan group nosodes speak of sluggish, congested livers and skins; Proteus of violent, often unconscious tension culminating in crises; Sycotic Co of chronic catarrh and fibrositis; Gaertner of nutritional and developmental derailment. Dysentery Co alone stands for conscious, anticipatory alarm in the autonomic field, with colon and pylorus as primary effectors.
When prescribed accurately, Dysentery Co often produces a gentle but decisive shift. The patient may report fewer emergency runs to the toilet, less abdominal churning before events, and a surprising ability to sit through meetings or exams without catastrophic thinking. Palpitations lessen, chest sensations feel less threatening, and sleep becomes less dominated by failure dreams. With the autonomic “volume” turned down, a more stable psychological baseline appears; at this point, the true constitutional remedy—be it Phos., Sulph., Lyc., Calc-ph., or another—usually becomes clear.
In essence, Dysentery Co is a terrain remedy for the autonomic gut–heart axis, where dysenteric history, anticipatory fear, bowel and chest sensations intertwine. It does not replace acutes like Acon. or Gels., nor deep polychrests, but prepares a nervous, dysenteric terrain to respond to them, and in many modern IBS–anxiety cases it is the missing link between psyche, flora and physiology.
Affinity
- Autonomic nervous system (sympathetic–parasympathetic balance) – Dysentery Co has a marked affinity for autonomic regulation: anticipatory nervous tension, “stage-fright” type anxiety, palpitations, precordial discomfort, and diarrhoea or pyloric spasm from anticipation. This permeates Mind, Heart, Stomach, Abdomen and Generalities.
- Pylorus and duodenum – Paterson emphasised selective action on the pylorus, producing spasm and retention of stomach contents, and duodenal ulceration from chronic nervous tension. This is central under Stomach and Abdomen and connects with modalities “worse anticipation” and “worse stress.”
- Colon and rectum (colitis, dysentery, IBS) – As the name suggests, Dysentery Co has a strong affinity for colon and rectum: mucus and blood in stools, colitis, post-dysenteric states and irritable bowel with cramping. Abdomen and Rectum sections express this fully.
- Small airways and upper respiratory tract – Several sources link Dysentery Co to small intestine and airways, with chronic nasal, ocular and pharyngeal mucosal irritation in anxious patients whose bowel symptoms alternate with respiratory complaints. Nose, Throat, Chest and Respiration show this.
- Cardiac area and chest (neuro-cardiac sensations) – A keynote is anticipatory discomfort in the cardiac area—tightness, pressure, pseudo-anginal pains arising from autonomic spasm rather than structural disease. This appears under Heart and Generalities.
- Sensorium and mental state (anticipatory fear, exam fear) – Dysentery Co acts on the sensorium with shyness, uneasiness, hypersensitivity to criticism, and anxiety before events: interviews, travel, examinations, performances. Mind and Dreams carry this keynote.
- Mucous membranes (nose, eyes, pharynx, bowel) – Inflammation of nasal, ocular and pharyngeal mucous membranes, often in parallel with pyloric and colonic symptoms, indicates a systemic mucosal affinity modulated by autonomic imbalance. Nose, Eyes, Throat and Abdomen all reflect it.
- “Colon–brain axis” (gut–emotional linkage) – Modern interpretations place Dysentery Co squarely on the gut–brain axis: anxiety-driven bowel dysfunction, post-infective IBS and autonomic digestive disturbance. This is woven through Mind, Stomach, Abdomen, Rectum and Generalities.
- Children and adolescents with exam fear and “gut nerves” – Dysentery Co’s pattern is particularly seen in school-age children and adolescents: anxiety about performance, fear of failing, loose stools before school or exams, and abdominal pain when facing change. Mind, Abdomen and Clinical Tips highlight this.
Better For
- Better once the anticipated event has begun or is over – The violent anticipatory tension and diarrhoea ease once the exam, journey or performance is underway; the patient calms as reality replaces imagined catastrophe. This pattern is echoed under Mind, Abdomen and Heart.
- Better with reassurance and clear information – Knowing what will happen, having a plan and feeling accompanied significantly soothes Dysentery Co patients; their “bloody terror” attenuates when uncertainty is reduced. Mind and Generalities reflect this.
- Better from warmth at the abdomen – Hot applications, warm drinks and gentle warmth over the stomach/abdomen ease pyloric and colonic spasm, paralleling other spastic remedies such as Coloc. Stomach and Abdomen both show this amelioration.
- Better after free stool (especially stress-diarrhoea) – Once the bowels have opened and the “nervous diarrhoea” has passed, mental and bodily tension often lessen, showing the gut as a chief vent for Dysentery Co. Abdomen, Rectum and Generalities link this with the autonomic discharge.
- Better with supportive company in stressful situations – The presence of a trusted person during anticipated events (exams, hospitals, travel) calms the dysenteric–autonomic response and helps stabilise pulse and bowels. Mind and Heart echo this.
- Better during moderate, steady activity – Gentle walking, pacing while waiting, and non-strenuous movement can dissipate nervous tension and reduce spasm, reminiscent of Gels. and Arg-n. Stomach, Heart and Generalities reflect this.
- Better from structured routines and predictable environments – Dysentery Co patients do better when days are structured, tasks are clear and surprises limited, reducing triggers for anticipatory tension. Mind and Generalities point to this.
- Better lying quietly after acute diarrhoeic episodes – After an episode of “nervous dysentery,” lying quietly, warmly covered, with minimal stimulation allows the autonomic system to reset. Abdomen, Rectum and Sleep sections show the restorative value of such rest.
Worse For
- Worse for anticipation (exams, interviews, travel, operations) – This is the central modality: anticipatory nervous tension leading to diarrhoea, cramping, palpitations and precordial discomfort, often hours before an event. Mind, Abdomen and Heart are dominated by this.
- Worse from fear of failure, criticism or “getting it wrong” – Hypersensitivity to criticism and dread of being judged or failing underlie much of the tension, and even imagined disapproval can trigger gut symptoms. Mind and Dreams mirror this.
- Worse before meals or soon after eating, when anxious – In nervous states, the pylorus goes into spasm; food feels “stuck,” with heaviness, nausea and delayed emptying, particularly under exam or work stress. Stomach and Generalities link this with pyloric affinity.
- Worse from coffee, stimulants and late nights – Stimulants aggravate sympathetic tone, intensifying palpitations, pyloric spasm and anxious insomnia; late nights and screen use similarly heighten reactivity. Mind, Heart and Sleep reflect this.
- Worse from sudden change of plan or environment – Any unforeseen demand—new school, new job, unexpected journey—can provoke a flare of diarrhoea, bowel colic and panic. Mind, Abdomen and Generalities highlight this.
- Worse from emotional shocks and bad news – Sudden shocks may bring immediate need for stool, shaking, tachycardia and chest tightness, with a picture reminiscent of Acon. yet more gut-focused and anticipatory in future episodes.
- Worse in crowded or closed spaces (offices, buses, exam halls) – Fear of not being able to escape to a toilet intensifies the autonomic response; exam halls, public transport and queues become torment. Mind, Heart and Generalities show this.
- Worse before menses (women) – In anxious, dysenteric women, anticipatory tensions around menses or gynaecological appointments may worsen cramps, diarrhoea and palpitations. Female, Abdomen and Heart reflect this.
- Worse in the early hours before an event (e.g. 3–6 a.m.) – Patients may wake early with a sense of impending doom, abdominal churning and urgent stools, which slowly settle after the event has begun. Sleep, Abdomen and Mind show this pre-dawn aggravation.
- Worse from recalling past humiliations or failures – Ruminating on earlier public failures or criticisms can trigger the same gut and cardiac sensations as present stress, demonstrating how memory alone can set off the Dysentery Co pattern. Mind and Dreams echo this.
Symptomatology
Mind
The mental picture of Dysentery Co is dominated by anticipatory nervous tension. Patients experience intense apprehension well before any event: examinations, speeches, journeys, operations, job interviews. Bach and later commentators described this tension as distinctly “anticipatory,” contrasting it with the more insidious, unrecognised tension of Proteus. The individual becomes hyper-vigilant, scanning for what could go wrong, with a powerful need to know the plan and control the outcome.
There is marked fear of failure and criticism. The Dysentery Co subject is hypersensitive to being judged, corrected or laughed at, and even mild criticism can evoke disproportionate shame and anxiety. Shyness and uneasiness, described by Bach, often coexist with a mask of competence; externally they may appear merely “nervous,” but internally they live in constant “what if?” scenarios. Children dread school tests, presentations or sports trials and may feign illness to escape such situations.
The gut is the barometer of their emotions: anxious thought immediately stirs abdominal churning, urging to stool or spasm at the pylorus. This differs from Gelsemium, whose anticipation produces paralysis and trembling with heavy eyelids, and from Arg-n., whose impulsive, hurried tendency coexists with fear of high places and narrow spaces. Dysentery Co shares Arg-n.’s “diarrhoea from anticipation,” but is less impulsive and more inwardly hyper-vigilant, with a more obvious colon/pylorus focus and autonomic chest discomfort.
Mentally, they are conscientious and often capable, but lose confidence under pressure. They rehearse conversations and events in advance, feel “butterflies in the stomach” escalating to cramps and diarrhoea, and may develop a phobic avoidance of situations where toilets are not readily accessible. Sleep is disturbed by racing thoughts about the coming day. In chronic states, a degree of mental fatigue and discouragement sets in; they begin to believe they will “never be normal.”
Case-style illustration: A bright 15-year-old, top of her class, developed intense diarrhoea and palpitations every exam morning. She described herself as “terrified of getting it wrong” and obsessed over the possibility of failing and “disappointing everyone,” with cramping and urgent stools from 5 a.m. until the exam began. Dysentery Co 200C led to reduction in anticipatory diarrhoea and a marked return of confidence, distinguishing it from Gels. and Arg-n. in this case. [Clinical]
Head
Head symptoms in Dysentery Co are largely secondary to autonomic tension. Anticipation may produce tight bands of tension around the head, frontal headaches with pressure over the brow and occipital stiffness. These headaches often precede exams, travel or interviews and may accompany pyloric spasm and palpitations.
Headaches can be throbbing or pressing, worse in closed, stuffy rooms (exam halls, offices) and from coffee or stimulants, and better in fresh air or after the stressful event. In chronic cases, patients complain of mental fatigue with heaviness in the head, difficulty concentrating and irritability, especially after a day of sustained anxiety or bowel disturbance.
There may be a tendency to dizziness on standing in anxious states, with a sense of “swimmy” vision if a panic attack threatens. This differs from the frank collapses of Gels. and the vertigo of Phos. or Kali-p., being more linked to autonomic lability than to structural disease.
Eyes
Ocular symptoms reflect general mucosal and autonomic imbalance: intermittent conjunctival irritation, redness and watering, particularly in nervous subjects who rub their eyes when tense. During prolonged concentration under stress (exams, screen work), eyes may feel strained and dry, then suddenly water when the tension peaks.
Lids may twitch from nervous fatigue, resembling Agar. or Zinc., but in a Dysentery Co context these tics accompany abdominal churning and anxious expectation. There can be transient blurring of vision during episodes of autonomic overactivity, with palpitations and a sense of unreality.
Ears
Ear symptoms are not prominent but may include a sense of blocked ears, pressure or mild tinnitus during anxious episodes, reflecting vascular and autonomic shifts. Some patients notice increased noise sensitivity on tense days, finding exam halls or crowded spaces oppressive.
In children with post-dysenteric or post-enteritis states, recurrent catarrh may extend to Eustachian tubes, with intermittent hearing dullness and earache, though Morgan and Gaertner nosodes usually cover more distinct otitis and malnutrition states.
Nose
The nose can be a secondary focus of mucosal irritation: chronic rhinitis, intermittent nasal blocking and thin mucus, often worse when the patient is anxious or run down. In some Dysentery Co types, emotional stress precipitates sneezing fits or “stress colds” where a minor chill under tension produces disproportionate mucosal response.
Alternation of diarrhoea with catarrhal episodes of nose and throat may be seen, and where this alternation is dramatic and linked to environmental changes, Mutabile may be more strictly indicated; yet in Dysentery Co, the bowels and autonomic heart sensations remain the foreground.
Face
The facial expression often betrays inner anxiety: tense jaw, tight lips, strained smile. Before anticipated events, the face may flush with sympathetic arousal or blanch with fear. Fine perspiration on upper lip and forehead appears during panic-like episodes.
In chronic dysenteric or post-infective states, features may become drawn, with dark circles under the eyes and a slight “pinched” look, especially if diarrhoea and weight loss persist. Compare to Phos. (more burning, haemorrhagic and sensitive), and to Argent-n. (more excitable, loquacious under nerves) for differentiation.
Mouth
Mouth symptoms reflect both GI and autonomic imbalance: dryness of mouth before or during anxious events, followed by excess saliva when nausea from pyloric spasm develops. There may be a “sour” or metallic taste preceding diarrhoea, and nervous subjects may clench teeth or bite lips during tension.
Aphthous ulcers may follow prolonged stress and digestive upset, but are not characteristic enough to be keynotes. Grinding of teeth at night can occur in schoolchildren who worry excessively about performance and discipline.
Teeth
Teeth do not form a central sphere for Dysentery Co, though in chronically anxious youngsters bruxism, increased caries from sugar used as “comfort food”, and discomfort on jaw clenching may appear. Dental procedures themselves can be major anticipatory triggers, with diarrhoea and palpitations the morning of an appointment; the nosode may be considered in such contexts when the broader pattern fits.
Throat
Throat sensations are classically “globus hystericus”: a lump in the throat, difficulty swallowing, or a choking sensation arising under emotion, not from structural disease. During anxiety attacks, patients may complain of tight, dry throat, frequent swallowing and urge to clear mucus, reflecting mucosal and autonomic involvement.
There may be mild pharyngitis or recurrent sore throats in chronically strained students or professionals, but, unlike Sycotic Co, massive tonsillar enlargement or adenoids are not central. The throat discomfort tends to wax and wane with emotional tension more than with infections.
Stomach
Here Dysentery Co is at its most characteristic. Bach and subsequent authors emphasised a “selective action on the pylorus causing spasm and retention of digestive contents,” with improvement in congenital pyloric stenosis and functional pyloric spasm. The patient complains of food “sitting like a stone” in the stomach, early satiety, nausea and pain in the epigastrium, especially under nervous strain.
Nervous dyspepsia predominates: even small meals before a stressful event provoke heaviness, cramping and a sense of arrested gastric emptying. Duodenal ulcer from chronic nervous tension belongs in the ambit of this nosode, though classical ulcer remedies (Arg-n., Kali-bi., Phos., Graph., Lyc.) must be differentiated; Dysentery Co is considered where emotional anticipation and dysenteric history are prominent.
The dyspeptic pain may radiate to the back and up into the chest, merging with precordial discomfort; patient cannot decide if it is stomach or heart pain. Warmth, small bland meals and reassuring circumstances ameliorate; coffee, rich foods, haste and examination conditions aggravate.
Abdomen
Abdominal symptoms centre on colitis and spastic colon. Colicky pains grip the lower abdomen, often with mucus and sometimes blood in the stool, echoing the dysenteric background. The urge for stool is sudden, often with a sense of “I must find a toilet now,” typically triggered by a stressful thought or situation.
Diarrhoea before events is a keynote: loose, sometimes explosive stools shortly before leaving home or entering an exam hall or clinic waiting room. Between attacks, bowel function may be relatively normal or pendulate between looseness and constipation. Gurgling, rumbling, and a “nervous churning” are felt, particularly from early hours of the morning when the patient lies thinking of the coming day.
Some patients have a history of bacillary dysentery or severe gastro-enteritis after travel, with never-complete recovery: since then they have been prone to IBS-like symptoms, flares of colitis and autonomic anxiety. Dysentery Co is well suited to such post-infective bowel syndromes where mental anticipation is conspicuous.
Urinary
Urinary manifestations are tangential: increased frequency and urgency during anxiety episodes, with normal urinalysis. The same autonomic overactivity that drives diarrhoea can provoke urgency to urinate, especially before leaving home, travelling or entering a stressful environment.
True cystitis, haematuria or structural urinary disease are uncommon in Dysentery Co, and their presence prompts differential consideration of Sycotic Co, Morgan group or specific organ remedies.
Rectum
Rectal symptoms include frequent small stools, tenesmus and a sense of incomplete evacuation. Stools may contain mucus and streaks of blood during acute colitis flares, but in chronic functional states, frank blood is less common than mucus and urgency.
There is often aggravation in the morning before work or school, with repeated visits to the toilet until the patient feels empty enough to leave the house. Fear of incontinence or of not finding a toilet is a major driver of anticipatory panic. This distinguishes Dysentery Co from purely inflammatory colitides where pathology dominates irrespective of mental state.
Male
In men, Dysentery Co appears in performance anxiety at work or in public life, with “gut nerves” and sometimes erectile difficulties tied strictly to anticipation rather than to underlying organic pathology. Palpitations and precordial pains before presentations or critical meetings contrast with general normal health at other times.
If a history of dysentery or severe diarrhoeal disease exists, the combination of post-infective IBS, exam-type anticipatory diarrhoea and chest autonomic symptoms makes Dysentery Co a strong candidate nosode, particularly where Arg-n. and Gels. have helped only partially.
Female
Women may show the same anticipatory bowels and pyloric spasm around job interviews, presentations or social events, with additional flares around menses or gynaecological appointments. Some women develop IBS-like colitis after dysentery in travel or pregnancy, never fully regaining bowel stability and becoming fearful of journeys and public events.
Premenstrual exacerbation of anxiety and diarrhoea is not uncommon. However, overt gynaecological pathology is less characteristic than in Sycotic Co or Morgan nosodes; Dysentery Co is more about autonomic gut–heart–mind interplay than about structural pelvic disease.
Respiratory
Respiration reflects anxiety: shallow breathing, sighing, difficulty taking a deep breath and occasional sensation of “air hunger” before events. Mild hyperventilation can occur in panic-like episodes, with tingling in extremities and dizziness.
Some patients develop a pattern where IBS-type bowel symptoms alternate or coexist with small airway issues—tight chest, tendency to bronchitis, throat clearing—particularly under stress. Dysentery Co has been noted in case series as linked with colon, small intestine and airway issues in such nervous subjects.
Heart
The heart sphere is crucial. Dysentery Co patients experience palpitations, tremulous pulse, and precordial awareness when anticipating events. They may describe a “racing heart,” irregular thumps or skipped beats, often with cold sweat and urgent need for stool.
This autonomic palpitatory state worsens with stimulants (coffee, energy drinks), late nights and rumination on feared situations. Typically, cardiology workups are normal; reassurance helps but does not fully prevent recurrence. The nosode acts at the autonomic level, helping to re-establish balance between sympathetic alarm and parasympathetic rest.
Chest
Chest symptoms revolve around autonomic discomfort. A keynote is “anticipatory discomfort in the cardiac area”: tightness, pressure, fluttering in the chest, sometimes described as a vice or grip, arising before dreaded events. These sensations often accompany epigastric heaviness, nausea and diarrhoea.
Dysentery Co is thus a remedy to consider in non-cardiac chest pain and “functional angina” where investigations are normal but anxiety and GI symptoms are obviously linked. Differentiation from Cactus (true constriction and heart pathology) and Gels./Arg-n. (less colon focus) is essential.
Back
Back symptoms are usually muscular and tension-based: tightness between scapulae, aching in neck and shoulders during stressful days, and a sense of weight in the upper dorsal spine when worried. These are secondary to autonomic arousal and prolonged sitting, rather than to structural disease as in Sycotic Co or Bacillus No. 7.
However, long-standing anxiety can produce functional postural issues and somatic focusing on the spine; the patient may fear serious disease though examination is normal. Dysentery Co helps particularly when spinal sensations clearly rise and fall with anticipatory tension.
Extremities
Extremity symptoms include cold hands and feet in anxiety, trembling of limbs and occasional paraesthesiae during hyperventilatory episodes. There may be restlessness of legs while waiting or sitting in stressful circumstances, akin to a light version of Arg-n.’s fidgetiness.
Cramps in calves or feet at night may follow dehydrating diarrhoeal episodes. After dysenteric illnesses, some patients complain of fatigue and heaviness in limbs, which improve as bowel function stabilises under correct treatment.
Skin
Skin symptoms are not central but may reflect autonomic and vascular lability: stress-induced flushing or pallor, cold clammy sweat on hands, and sometimes transient urticaria under strong emotion.
Post-dysenteric malabsorption may lead to dry, rough skin, weight loss and pallor, but these are not specific to Dysentery Co. When skin alternates with asthma or bowel, Mutabile or Gaertner often take precedence, with Dysentery Co as a consideration if anticipatory tension dominates.
Sleep
Sleep is disturbed by anticipatory thoughts and recurring “what if?” scenarios. Patients wake in the early hours (3–5 a.m.) with churning abdomen, dread of the coming day and sometimes urgent need for stool. It may take hours to return to sleep, leading to daytime fatigue.
Children fret in bed about school tests, social situations or disciplinary encounters; they may sleep lightly, wake repeatedly and seek reassurance. Adults replay conversations or pre-live upcoming events, experiencing palpitations and bowel rumbling even while lying still. Once the stressful period passes, sleep usually improves, underscoring the centrality of anticipation.
Dreams
Dreams in Dysentery Co revolve around examinations, being unprepared, failing, being ridiculed or publicly humiliated. Patients may dream they arrive late, sit the wrong exam, or stand in front of an audience unable to speak, waking in fright with pounding heart and urgent stool.
Other dreams include travel disasters (missing trains, planes, losing tickets) and being trapped in places without toilets. These dreams often precede real-life events and mirror the daytime preoccupations, giving additional confirmation of the nosode when accompanied by bowel and cardiac autonomic symptoms.
Fever
Dysentery Co is not primarily a high-fever remedy. Fever appears chiefly during acute dysenteric or colitic episodes and in post-infective phases; however, once the acute infection is resolved, low-grade temperature or a “feverish feeling” may accompany flare-ups of anxiety and bowel disturbance.
In chronic IBS-type cases, fever is usually absent; its presence should prompt investigation for organic colitis, infection or inflammatory bowel disease, with Dysentery Co considered only in the functional overlay.
Chill / Heat / Sweat
Chilliness during anxiety is common—cold, clammy hands, shivering despite warm surroundings. Heat may manifest as sudden hot flushes during panic-like episodes, particularly in the face and chest. Sweats are often cold and clammy rather than hot and profuse, especially on palms, soles and forehead.
After diarrhoeal attacks, patients may feel alternately chilled and heated, reflecting autonomic swings; lying quietly, warmly covered usually restores balance.
Food & Drinks
Appetite is variable, falling sharply under stress. Some patients cannot eat before exams or interviews without nausea; others eat compulsively for comfort, then suffer dyspepsia and diarrhoea. Spicy and rich foods, coffee and alcohol frequently aggravate, especially in anxious periods.
Cravings for sweets and refined carbohydrates may be present but carry no strong keynote weight. A history of traveller’s diarrhoea or dysentery following questionable food or water is often part of the background. Hydration and simple, bland diets during flares support the nosode’s action.
Generalities
In general, Dysentery Co presents a picture of anticipatory autonomic storm centred on the gut and heart area. The chief themes are anxiety, fear of failure and criticism, heightened sensitivity to impending events, and a gut that reacts immediately to emotional stimuli with pyloric spasm, colitis and diarrhoea.
This nosode belongs to the “autonomic–apprehensive tension” group of bowel nosodes, contrasting with the “synovial–mucous irritability” of Sycotic Co, the “portal–skin congestion” of Morgan, the “vascular–storm” of Proteus, the “nutrition–malabsorption” of Gaertner, and the “senile weakness” of Bacillus No. 7. It is especially suited to thin, anxious individuals, often with a history of dysentery or severe gastro-enteritis, whose nervous systems have never fully recovered and who now show IBS-like bowel behaviour tightly linked to stress.
Autonomic dysregulation bridges gut, heart and mind: palpitations, tight chest, diarrhoea, trembling and clammy sweat form a unified response to perceived threat. Modern “gut–brain axis” thinking fits neatly here: Dysentery Co acts where emotional triggers, microbiome changes and enteric nervous system hyper-reactivity interact. As the nosode works, anticipatory storms become less frequent and less intense, bowels stabilise, and the patient can face previously dreaded situations with more equanimity, at which point constitutional remedies show clearer profiles.
Differential Diagnosis
Anticipatory Anxiety & “Stage Fright”
- Dysentery Co vs Argentum nitricum – Both have diarrhoea from anticipation, fear of failure and anxiety before events. Arg-n. is more impulsive, hurried, and theatrically anxious, often craving sweets; Dysentery Co is more inwardly hyper-vigilant, with stronger dysenteric history, pyloric spasm and autonomic precordial discomfort.
- Dysentery Co vs Gelsemium – Gels. anticipates with weakness, trembling, heaviness and desire to be left alone; bowels may be loose but mental paralysis predominates. Dysentery Co anticipates with hyper-vigilance, “bloody terror,” pyloric spasm and IBS-type diarrhoea, remaining mentally alert but overwhelmed.
- Dysentery Co vs Kali-phos. – Kali-p. covers nervous exhaustion and exam anxiety with prostration, but lacks the marked dysenteric colon–pylorus picture and anticipatory chest discomfort of Dysentery Co.
IBS / Colitis / Post-dysentery
- Dysentery Co vs Colocynthis – Both have colicky abdominal pains and diarrhoea. Coloc. pains are cramping, doubled-up, better hard pressure and bending double; Dysentery Co pains are closely tied to anticipation, with less dramatic doubling-up and more autonomic chest and pyloric features.
- Dysentery Co vs Mercurius corrosivus – Merc-cor. has severe dysenteric stools with intense burning, tenesmus and blood; Dysentery Co is more chronic and functional, with milder blood/mucus and strong autonomic and anticipatory overlay.
- Dysentery Co vs Morgan-pure – Morgan-pure relates to portal congestion, skin eruptions and bilious dyspepsia with Sulphur-like traits; Dysentery Co to colon–pylorus spasm, IBS and autonomic tension. Portal and skin issues point to Morgan; anticipatory gut and heart to Dysentery Co.
Autonomic Chest / Non-cardiac Chest Pain
- Dysentery Co vs Cactus grandiflorus – Cactus has iron bands, true cardiac pathology, congestion; Dysentery Co has anticipatory, functional precordial discomfort with normal investigations and clear gut link.
- Dysentery Co vs Aconitum – Acon. covers sudden intense fear of death and tachycardia after shock; Dysentery Co is more chronic, anticipatory, linked to performance and diarrhoea, with less violent onset.
Bowel Nosode Group
- Dysentery Co vs Proteus – Both involve nervous tension. Proteus tension is insidious, unrecognised, exploding suddenly into crises (ulcer, stroke-like episodes); Dysentery Co’s tension is consciously felt and anticipatory, manifesting as IBS-type diarrhoea and mild chest pains.
- Dysentery Co vs Sycotic Co – Sycotic Co focuses on mucous and synovial membranes, chronic catarrh and fibrositis; Dysentery Co on colon, pylorus and autonomic anxiety. Warts, rheumatism and damp aggravation point to Sycotic Co; examination gut and precordial tension to Dysentery Co.
- Dysentery Co vs Gaertner – Gaertner is a malnutrition, malabsorption and multiple food intolerance nosode; Dysentery Co is more about autonomic anticipatory diarrhoea than about profound undernutrition.
- Dysentery Co vs Mutabile – Mutabile centres on alternation of skin, lung and bowel symptoms, often with Puls. traits. Dysentery Co has a more continuous gut–autonomic pattern, with less striking alternation and more exam-type fear.
Remedy Relationships
- Complementary: Argentum nitricum – Shares diarrhoea from anticipation and performance anxiety. When Arg-n. only partially relieves, especially in post-dysenteric IBS with chest autonomic sensations, Dysentery Co may clear the bowel-flora layer and allow Arg-n. to act more fully.
- Complementary: Gelsemium – In some students and performers, Gels. helps physical prostration while Dysentery Co addresses deeper IBS-type anticipatory diarrhoea and pyloric spasm. They may be needed sequentially as layers of the same constitutional pattern.
- Complementary: Phosphorus – Phos. often follows Dysentery Co in thin, sensitive, haemorrhage-prone individuals once the dysenteric flora pattern and autonomic gut storms have settled.
- Complementary: Tuberculinum – In tubercular-tinged adolescents with restlessness, change-seeking and recurrent post-infective bowel issues, Dysentery Co may prepare the ground for Tub., clarifying the tubercular picture.
- Complementary (bowel nosode sequence): Morgan-pure, Sycotic Co, Bacillus No. 7 – In chronic multi-system cases, Dysentery Co may appear in a sequence of bowel nosodes as stool flora and symptom picture evolve; it particularly bridges autonomic gut tension with Morgan or Sycotic-type catarrh and musculo-skeletal issues.
- Follows well: Acute dysentery remedies (Merc-cor., Pod., Colch.) – After acute dysentery has been controlled by appropriate remedies and orthodox care, Dysentery Co may follow to address lingering functional colitis and anticipatory bowel behaviour.
- Follows well: Acon., Ign., Kali-p. – In patients whose acute shock and grief states have settled but left behind chronic autonomic gut over-reactivity, Dysentery Co may follow these acute mental remedies to stabilise the gut–brain axis.
- Precedes well: Constitutional polychrests (Phos., Sulph., Lyc.) – In many chronic IBS–anxiety cases, constitutional remedies only act fully after Dysentery Co has reorganised the bowel flora terrain and quieted the anticipatory autonomic overdrive.
Clinical Tips
- Think of Dysentery Co in “exam IBS” – Students with loose stools, cramps and “bloody terror” before tests or performances, especially if they also fear criticism and failure despite being capable. Dysentery Co 200C or 1M as an intercurrent between constitutional remedies can markedly reduce anticipatory diarrhoea.
- Post-dysenteric IBS – After bacillary dysentery or severe traveller’s diarrhoea, some patients develop chronic IBS with stress-triggered flares. Where colon–heart–mind linkage is clear, Dysentery Co in medium–high potency, given sparingly, can help reorganise bowel flora and autonomic patterns, followed by constitutional therapy.
- Functional chest pain with normal investigations – In patients with recurrent precordial pains and palpitations centred on anticipation, with normal cardiology workups and concurrent IBS, Dysentery Co is worth considering as part of the differential with Cactus, Acon. and Arg-n.
- Potency and repetition – Following Paterson’s principles for bowel nosodes, higher potencies suit cases where mental generals (anticipation, criticism sensitivity) predominate; lower potencies when pathology (colitis, ulcer) is stronger. Repetition is cautious; many authors advise not repeating the same bowel nosode more often than every few weeks unless clear indications arise.
- Case pearl (student) – A 17-year-old boy, history of severe gastro-enteritis aged 12, now suffers diarrhoea and cramping every exam morning, with icy hands, palpitations and fear of disappointing his parents. Arg-n. and Gels. helped partially. Dysentery Co 200C, single dose, given one month before final exams, was followed by reduced diarrhoea and calmer mood; Arg-n. then sufficed acutely for minor nerves.
- Case pearl (professional) – A 38-year-old lawyer with normal cardiac tests had episodes of chest tightness and diarrhoea before court appearances and presentations, with obsessive fear of making mistakes. After Dysentery Co 1M, there was a steady decline in pre-hearing diarrhoea and chest symptoms; a subsequent Phos. prescription addressed residual sensitivity and fatigue.
- Case pearl (post-dysentery) – A 45-year-old woman, after dysentery contracted abroad, developed chronic IBS and terror of travel. Acute colitis was long resolved, but any journey provoked diarrhoea from the moment she packed. After Dysentery Co 30C, repeated at intervals, her bowel stability improved and she was able to undertake short trips without accidents, later managed constitutionally.
Selected Repertory Rubrics
Mind
- Mind; anxiety; anticipation; diarrhoea with – Intense apprehension before events with loose stools.
- Mind; fear; failure; examinations; of – Fear of getting it wrong, failing tests, disappointing others.
- Mind; sensitive; criticism; to – Hypersensitive to criticism, easily hurt and ashamed.
- Mind; shyness; uneasiness; social situations – Shy, uneasy in public or evaluative situations.
- Mind; fear; public speaking; diarrhoea before – Loose stools and palpitations preceding presentations.
Head
- Head; pain; tension; frontal; anticipation before – Frontal tension headache in exam or interview anticipation.
- Head; heaviness; mental fatigue; anxiety with – Heavy, tired head after a day of autonomic overdrive.
Stomach / Abdomen / Rectum
- Stomach; spasm; pylorus; nervous; anticipation from – Pyloric spasm, food retained, from emotional strain.
- Stomach; ulcer; duodenal; nervous; tension from – Duodenal ulcer linked to chronic anticipatory stress.
- Abdomen; colic; anxiety; during; diarrhoea with – Griping colic accompanying exam-type diarrhoea.
- Rectum; stool; mucus; blood; colitis; chronic – Mucus and some blood in stools in chronic colitis syndromes.
- Rectum; diarrhoea; anticipation from; examinations, interviews before – Loose stools repeatedly before evaluative events.
Heart / Chest
- Heart; palpitation; anxiety; anticipatory – Palpitations in expectation of future events.
- Chest; pain; precordial; functional; anxiety; from – Precordial discomfort with normal cardiac tests, linked to stress.
Respiration
- Respiration; difficult; anxiety; before events – Shortness of breath, sighing, air hunger under anticipatory stress.
Sleep / Dreams
- Sleep; waking; early; anxiety; of coming day – Wakes 3–5 a.m. worrying about future events.
- Dreams; examinations; being unprepared – Dreams of failing or being unready for tests, with fright.
- Dreams; humiliation; public – Dreams of being laughed at, criticised or exposed in public, with gut sensations.
Generalities
- Generalities; anticipation; ailments from – Wide range of complaints (bowel, heart, sleep) from anticipatory fear.
- Generalities; dysentery; after; never well since – Chronic IBS and anxiety states following dysentery.
- Generalities; autonomic; imbalance; gut–heart axis – Symptoms reflecting dysregulation of autonomic control across gut and heart.
References
Bach E — “The Relation of Vaccine Therapy to Homoeopathy” (British Homoeopathic Journal, 1920): early description of bowel flora, autogenous vaccines and transition to potentised bowel nosodes.
Paterson J — The Bowel Nosodes (mid-20th century; reprint editions): detailed accounts of Dysentery Co, its anticipatory nervous tension keynote, pyloric action and clinical indications.
Sharma C P, Ambwani M, Saraswat K — “Bowel Nosodes – A Boon to Homoeopathy” (The Homoeopathic Heritage, 2021): historical overview, preparation, miasmatic analysis and tabular summary including Dysentery Co group themes.
Remedia Encyclopaedia — “Bowel Nosodes: Dysentery Co.”: concise clinical summary of keynotes (anticipatory nervous tension, pyloric spasm, duodenal ulcer, cardiac area discomfort).
Paterson J — “The Role of the Bowel Flora in Chronic Disease” (British Journal of Nutrition, 1949): discusses disturbed bowel flora in chronic illness and mentions Dysentery Co as therapeutically useful when totality matches.
Qjure Database — “Bowel Nosodes: Dysentery Co.”: modern synthesis of associated remedies, bodily system grouping (autonomic–apprehensive tension) and clinical affinities.
Kshirsagar I et al. — “Utility of Bowel Nosodes in the Treatment of Chronic Diseases: A Case Series” (2023): includes Dysentery Co among frequently used bowel nosodes in complex chronic cases.
Sage Journals Case Study — “Homeopathic Bowel Nosode Remedies for Gut–Brain Axis Disorders” (2018): links Dysentery Co with colon, small intestine and airway issues, and describes its anxious, anticipatory profile.
Elements of Health Clinic Notes — “Gut Health: Bowel Nosodes” (2017): clinical commentary emphasising Dysentery Co as an anxiety/“bloody terror” nosode with diarrhoea from fear of getting it wrong.
Zenith Research — “Understanding Bowel Nosodes Through Diagrammatic Representation” (2022): includes diagrammatic mapping of Dysentery Co indications in various chronic conditions.
CORE Education — “Systems & Symbiosis: The Bowel Nosodes Reappraised” (c. 2007): modern interpretation of bowel nosodes in chronic disease, gut–brain axis, and clinical methodology, including Dysentery Co.
Disclaimer
Educational use only. This page does not provide medical advice or diagnosis. If you have urgent symptoms or a medical emergency, seek professional medical care immediately.