Cholinum
Substance Background
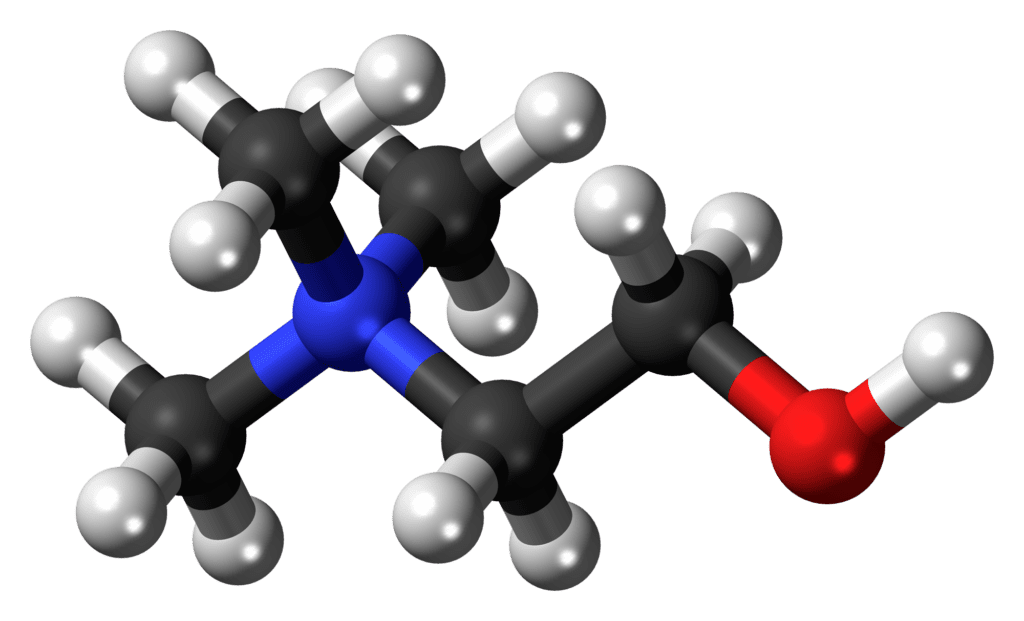
Cholinum (choline) is a nitrogenous, vitamin-like nutrient (often grouped historically with the “B-complex” factors) and a fundamental building block in human physiology. [Clinical] It stands at a crossroads of nerve signalling, membrane structure, and methylation chemistry: it is the well-known precursor of acetylcholine (the great parasympathetic and memory-linked neurotransmitter), and it is also incorporated into phosphatidylcholine and sphingomyelin, which are essential constituents of cell membranes, myelin, and bile. [Clinical] Choline is further linked to methyl donation through its oxidation to betaine, touching liver metabolism, homocysteine handling, and the wider “chemical stamina” of the organism. [Clinical] In homeopathic pharmacy, Cholinum is prepared by trituration and potentisation; as a modern substance it does not belong to the classical Hahnemann-era proving canon, so its use must be anchored in careful observation, clear modalities, and repeated clinical confirmation rather than routine diagnosis-based prescribing. [Hahnemann], [Kent]
From a toxicologic standpoint, choline in pharmacologic quantities may produce a characteristic cluster—gastrointestinal upset, sweating, hypotension, and a fishy body odour—features which, in homeopathic thinking, can help illuminate the direction of a remedy’s possible sphere, without claiming an extensive proving. [Toxicology], [Hughes] The remedy picture below is therefore written as a disciplined synthesis: a “cholinergic-membrane-liver” pattern, expressed through mind, nerves, digestion, bile, and fatigue, to be used only when the individualising features strongly agree. [Hahnemann], [Vithoulkas]
Proving Information
No classical proving symptoms recorded in the early Hahnemann-era sources. [Hahnemann] Cholinum belongs to modern practice, where its themes are inferred through contemporary toxicology, physiological correspondence, triturations where available, and clinical confirmation, with special caution to avoid diagnostic routine prescribing. [Hughes], [Teixeira], [Vithoulkas]
Remedy Essence
Cholinum is the picture of a system that has lost its metabolic and nervous rhythm: the mind becomes foggy when the body is poorly fed, the emotions become irritable when sleep is thin, and the digestion becomes heavy when the person tries to compensate with rich foods, stimulants, and late routines. [Clinical], [Boger] The patient’s complaint is not only “tiredness,” but a sense of sluggish signalling: the brain cannot hold attention, the memory slips, and the whole person feels thickened, as though the vital force is labouring through sticky mediums. [Kent], [Clinical]
The genius of the remedy lies in its tight linkage between cognition and digestion. When meals are irregular, the mind collapses; when food is taken regularly, the mind steadies. When fats are heavy, the abdomen and head become loaded; when the evening is light and earlier, sleep improves and the next day’s mind is clearer. [Clinical], [Hughes] This rhythm dependence gives a practical set of confirmatory signs: worse from fasting, worse from rich greasy foods, worse from sleep loss, worse in close heated rooms; better from regular nourishment, rest, quiet, fresh air, and warmth. [Kent], [Boger]
In temperament, Cholinum is not primarily dramatic; it is often weary and easily overtaxed. Irritability appears as the voice of depletion, not as a fixed character flaw: the person becomes snappy when hungry or tired and regrets it afterwards, improving once they are fed and rested. [Clinical], [Vithoulkas] The sycotic colouring can show as “stagnation”: the sense of being clogged, heavy, and slow to clear, physically and mentally, with a tendency to accumulate heaviness when routine slips. [Kent], [Sankaran]
When Cholinum acts curatively, the patient often describes a return of inner steadiness: hunger no longer produces emotional collapse, digestion becomes lighter, sleep becomes more restorative, and the mind can work without constant re-feeding or stimulant pushing. This global rhythm restoration, rather than a single isolated symptom change, is the true signature that the remedy has met the case. [Hahnemann], [Vithoulkas]
Affinity
- Central and autonomic nervous system (cholinergic tone): states of mental fog, poor attention, and autonomic imbalance (dryness vs sweating, constipation vs looseness), especially when fatigue worsens the whole picture (see Mind, Sleep, Generalities). [Clinical], [Kent]
- Memory and executive function: difficulty sustaining focus, word-finding weakness, “blankness” after mental exertion; better from rest and quiet (see Mind, Head). [Clinical], [Boger]
- Liver and bile physiology: heaviness after fats, nausea, pale or sluggish digestion themes, a sense of hepatic “load” (see Stomach, Abdomen, Food and Drink). [Clinical], [Hughes]
- Cell membranes / myelin context: neurological sensitivity after strain, convalescence, or chronic depletion; “thin reserves” and slow recovery (see Generalities). [Clinical], [Vithoulkas]
- Gut motility and secretions: constipation from sluggish peristalsis, or conversely looseness when the system is overstimulated; symptoms fluctuate with stress and diet (see Rectum). [Clinical], [Kent]
- Sweat and odour (toxicologic echo): episodes of clammy perspiration, body odour changes, and faintness during digestive upset (see Perspiration, Generalities). [Toxicology], [Hughes]
- Sleep–wake regulation: unrefreshing sleep with morning fog, or wakefulness from mental activity; strong link between sleep loss and cognitive failure (see Sleep). [Kent], [Vithoulkas]
- Nutrition-linked weakness: “runs on fumes” when meals are irregular; marked worsening from fasting or skipping breakfast (see Food and Drink, Generalities). [Clinical], [Boger]
Better For
- Better from quiet and sensory reduction (general): mind clears when noise and bustle stop; this tallies with the sensory overload noted under Mind and Head. [Kent], [Clinical]
- Better from sleep, even short naps (general): a nap “reboots” the mind; morning fog lessens after truly restorative sleep (see Sleep). [Kent], [Clinical]
- Better from fresh air and gentle walking (general): mild movement clears heaviness without exhausting; unlike overexertion which drains (see Generalities). [Boger], [Clinical]
- Better from regular meals (general/stomach): steadier cognition and less faintness when meals are punctual; worse when skipping food (see Food and Drink). [Clinical], [Vithoulkas]
- Better from warmth (general): chilly sluggishness and abdominal tightness ease in warmth; the system “moves” better (see Chill / Heat / Sweat). [Boger], [Clinical]
- Better from lying on the right side (abdomen): hepatic heaviness and nausea ease in certain patients, suggesting a liver-bile correspondence (see Abdomen). [Clinical], [Hughes]
- Better from gentle pressure to abdomen (abdomen): abdominal unease and rumbling settle from light support; not violent colic (see Abdomen). [Clinical], [Boger]
- Better from avoiding heavy fats late (food): digestion steadies when fatty meals are reduced at night; sleep becomes less disturbed (see Food and Drink, Sleep). [Clinical], [Vithoulkas]
Worse For
- Worse from mental exertion (mind/head): concentration quickly collapses; after study the mind becomes muddy and irritable (see Mind). [Kent], [Boger]
- Worse from sleep deprivation (general): even one late night worsens fog, digestion, and emotional steadiness (see Sleep, Generalities). [Kent], [Vithoulkas]
- Worse from rich or greasy food (stomach/liver): heaviness, nausea, and sluggishness after fats; “liver-loaded” feeling (see Stomach, Abdomen). [Hughes], [Clinical]
- Worse from irregular meals or fasting (general): shaky weakness, irritability, and head fog when meals are skipped (see Food and Drink). [Clinical], [Boger]
- Worse from alcohol (general): worsens sleep quality and next-day mental clarity; digestive heaviness intensifies (see Food and Drink). [Clinical], [Vithoulkas]
- Worse in close, heated rooms (general/head): fog and head heaviness worsen in stale air; better outside (see Head). [Boger], [Kent]
- Worse from emotional strain and worry (mind): rumination “burns out” attention; digestive symptoms follow mental stress (see Mind, Stomach). [Kent], [Vithoulkas]
- Worse late afternoon or evening crash (general): cognitive stamina fails later in the day; irritability and sluggish digestion increase (see Sleep, Generalities). [Boger], [Clinical]
Symptomatology
Mind
Cholinum presents as a mind that feels underpowered and poorly regulated, as though the “signal” is weak and the background noise too loud. [Clinical] There is often a striking inability to sustain attention: the patient reads a page and must re-read it, loses the thread mid-sentence, and becomes irritated at their own mental failure; this is worse from mental exertion as already noted in the modalities. [Kent], [Boger] The mind may alternate between dullness and restless striving, a state of “trying to push through” that only worsens the fog, until the person finally withdraws into quiet, where the mind partially clears (better from quiet). [Kent], [Clinical] Memory weakness is frequently functional rather than degenerative: names, words, and plans slip, especially when meals are irregular or sleep has been poor; this directly reflects the nutrition-linked and sleep-linked affinities (see Food and Drink; Sleep). [Clinical], [Vithoulkas]
Emotionally there may be a mild despairing tone, not dramatic, but a weary sense of being “too slow,” with self-reproach; the patient becomes overly sensitive to demands and interruptions. [Clinical] Anxiety often arises from physiological instability: hunger, tiredness, and digestive heaviness produce a reactive anxiousness, rather than purely psychological fear, and it improves when the body is steadied by rest and regular meals. [Clinical], [Hahnemann] A characteristic irritability can appear with sensory overload—noise, crowds, fast conversation—because the brain cannot filter stimuli, and this oversensitivity worsens notably in close, heated rooms (worse from stuffy air). [Kent], [Boger] Micro-comparison: Kali-phos. has classic nervous exhaustion and irritability; Cholinum is suspected when the exhaustion is tightly linked to digestion, irregular meals, and a “liver-bile heaviness” feeling, with strong improvement from nutritional rhythm. [Boger], [Clinical] Case-note style: a patient who becomes foggy, snappy, and forgetful when breakfast is missed, then improves markedly after food and a short nap, may confirm the Cholinum pattern if the whole totality agrees. [Clinical], [Vithoulkas]
Head
The head symptoms often feel like weight and congestion without true inflammation: dull pressure, frontal or vertex heaviness, and a sense that the brain is “thick” or “greasy,” worse after prolonged thinking and worse in close rooms, better in fresh air. [Boger], [Kent] Headache may accompany digestive heaviness: the head feels loaded after rich food, especially late, and the next day brings a dull fog; this links Head to the liver-bile affinity already noted (see Food and Drink). [Clinical], [Hughes] Dizziness can be faint, more like light-headedness from irregular meals than true vertigo; it is worse from fasting and better after eating, again echoing the nutrition-linked modality. [Clinical] Some report a curious morning fog: the head wakes slowly, and only after a routine of food, movement, and time does clarity return; this strongly ties Head to Sleep and Generalities. [Clinical], [Vithoulkas]
Sensitivity to noise and bustle is common: the head “cannot bear” too much input when foggy, and quiet helps; this is not merely temperament, but a threshold phenomenon of the nervous system. [Kent], [Clinical] Micro-comparison: Nux-v. may have head pressure from dietary excess and irritability; Cholinum is less driven and more “depleted-sluggish,” with stronger dependence on regular meals and sleep to restore. [Kent], [Clinical] Another comparison: Chelidonium has marked hepatic headache with right-sided and scapular correspondence; Cholinum may resemble hepatic heaviness yet shows a more “cognitive-metabolic” overlay with fog and attention failure as central, rather than the strong biliary pain picture. [Clarke], [Hughes] When the remedy is correct, the first improvement is often a clearer morning head and less crash after ordinary mental work, rather than mere pain relief. [Hahnemann], [Vithoulkas]
Eyes
The eyes in Cholinum cases often reflect processing fatigue rather than local ocular disease. [Clinical] Reading becomes effortful: the eyes may blur, but the patient’s main complaint is that the brain cannot interpret quickly; words seem to “slide off” the mind. [Clinical] Screens aggravate, especially rapid scrolling or visually busy environments; the symptom is often accompanied by head heaviness and irritability, matching the modalities (worse from stimulation; better from quiet). [Kent], [Clinical] The eyes feel tired late afternoon or evening, coinciding with the general crash, and are better after sleep. [Clinical], [Vithoulkas] Light sensitivity can occur when the nervous system is overtaxed, but it is typically part of the broader sensory intolerance. [Kent]
Micro-comparison: Nat-m. has headaches from eye strain with emotional themes; Cholinum’s eye strain is more bound to metabolic rhythm, fatigue, and digestive heaviness, with a strong “better after food and rest” signature in some patients. [Kent], [Clinical] Another comparison: Arg-n. may be overwhelmed by sensory input and have anticipatory strain; Cholinum is less anticipatory and more physiologically depleted, with fog and heaviness predominating. [Kent], [Clinical] Practical observation as obstacle-to-cure: late-night screen use worsens sleep and thereby worsens eye-brain fatigue; addressing this may be necessary to see clean remedy action. [Hahnemann], [Vithoulkas] Improvement is suggested when reading becomes easier, screen tolerance increases without headache, and the evening eye-fatigue lessens as sleep becomes more restorative. [Clinical], [Vithoulkas]
Ears
Ear symptoms are usually secondary, yet many Cholinum patients show a notable intolerance of noise, as though the auditory input penetrates too deeply and rapidly exhausts the mind. [Kent] Crowds, many voices, and background sound can provoke irritability and confusion, and the person seeks quiet; this matches the Mind and Head picture and the “better in quiet” modality. [Kent], [Clinical] Mild tinnitus may appear during stress and sleep deprivation, not as a primary ear pathology but as a nervous-system accompaniment. [Clinical] There may be a sensation of pressure in the ears when the head feels heavy after rich foods or late meals, linking the sensory complaint to the digestive-biliary axis. [Clinical]
Micro-comparison: Nux-v. is highly noise-sensitive with anger and overstimulation; Cholinum is more “foggy and heavy,” less hot-tempered by nature, more easily exhausted and dulled by noise. [Kent], [Clinical] Kali-phos. may show noise intolerance in nervous exhaustion; Cholinum is suspected when the exhaustion is clearly tied to meal rhythm, digestive heaviness, and a “metabolic slump” pattern. [Boger], [Clinical] When the remedy acts, the patient can tolerate ordinary sound without becoming mentally scattered, and the desire to withdraw into silence becomes less urgent. [Clinical], [Vithoulkas]
Nose
Nasal symptoms are not a dominant sphere, yet smell and air quality can matter. [Clinical] Stale, heated rooms aggravate fog and headache, and the patient may feel mentally “stifled,” craving open air, which is a useful general modality. [Boger], [Kent] Strong odours can provoke nausea when digestion is sluggish, linking Nose to Stomach by a reflex sensitivity rather than by coryza. [Clinical] Some patients describe a dry nasal feeling during depleted states, while others show watery discharge when the system is overloaded; these fluctuations should be weighed only as concomitants. [Hahnemann]
Micro-comparison: remedies with strong nasal catarrh keynotes should be chosen when the nose is central; Cholinum is only considered when nasal complaints are clearly subordinate to cognitive-metabolic and hepatic themes. [Kent] If the patient improves, the chief sign is not “a better nose,” but better tolerance of air quality and less staleness aggravation as the general state steadies. [Clinical], [Vithoulkas]
Face
The face often carries the imprint of fatigue: a dull, tired look, slight puffiness in some, and an expression of “mental heaviness.” [Clinical] Facial colour may fluctuate with digestive load: pallor with faintness when meals are missed, and a heavier, sallow tone during sluggish digestion, echoing the liver-bile affinity. [Clinical], [Hughes] There may be jaw tension from effortful concentration, which worsens under pressure and improves when the mind rests, matching the modalities. [Clinical] In some cases, perspiration of the face appears during digestive upset or stress (a toxicologic echo of sweating), and is relieved by fresh air and rest. [Toxicology], [Clinical]
Micro-comparison: Chelidonium can show sallow face with liver involvement; Cholinum differs by the prominence of fog, memory weakness, and sleep-linked crash patterns. [Clarke], [Clinical] When the remedy acts, the face looks clearer and less drawn, not by cosmetics, but by restored nervous steadiness and improved sleep quality. [Clinical], [Vithoulkas]
Mouth
The mouth symptoms often express sluggishness: dry mouth in states of stress and fatigue, or a coated tongue when digestion is heavy, particularly after fats. [Clinical], [Hughes] Taste may be dull, and appetite becomes irregular: either loss of appetite with heaviness, or cravings for quick fuel when the mind is foggy. [Clinical] Word-finding difficulty can feel “in the mouth” as hesitation, yet the problem is cortical retrieval rather than tongue paralysis; it worsens when tired and improves after rest and food. [Clinical] Salivation may increase during nausea episodes, reflecting an autonomic shift; this is an important concomitant when present, and it echoes the cholinergic theme without claiming a full proving. [Clinical]
Micro-comparison: Merc. has salivation with offensive mouth and ulceration; Cholinum salivation, when present, is more episodic and tied to nausea and metabolic swings, not to septic mouth pathology. [Kent], [Clinical] Improvement is seen when the tongue clears, appetite becomes steadier, and speech hesitation reduces as the general fog lifts. [Clinical], [Vithoulkas]
Teeth
Teeth symptoms are not central. [Hahnemann] If present, they often relate to bruxism from stress and fatigue, or sensitivity during depleted states; these should be interpreted cautiously as concomitants rather than prescribing anchors. [Clinical] When the remedy is correct, such symptoms improve indirectly as sleep deepens and nervous tension reduces. [Clinical], [Vithoulkas]
Throat
The throat may feel tight during mental strain, as though the body holds its breath while thinking. [Clinical] Swallowing can be slightly difficult during nausea or autonomic imbalance, and improves with calm, warmth, and quiet. [Clinical] Some patients complain of a lump sensation when worried and fatigued; this is not the dramatic hysterical globus, but a dull constriction linked to exhaustion. [Clinical] There may be throat dryness in stale rooms and improvement in fresh air, repeating the general modality. [Boger], [Kent]
Micro-comparison: Ign. has globus with contradictions and strong emotional drama; Cholinum’s throat sensations are typically fatigue-linked and improve with physiological stabilisation (food, rest, sleep). [Kent], [Clinical]
Stomach
The stomach in Cholinum is often a centre of heaviness and slow processing. [Clinical] There is fullness after rich foods, nausea after fats, and a sense that digestion “stops,” especially late in the day; this aggravation from greasy food is a main confirmatory modality. [Hughes], [Clinical] Missing meals produces a different state: weakness, irritability, light-headedness, and brain fog, often relieved promptly by eating; this creates a picture where the mind and stomach rise and fall together. [Clinical] Appetite may be capricious: the patient wants stimulation but is punished by it (coffee, alcohol), which then worsens sleep and next-day fog; this is a classic obstacle-to-cure scenario in modern lifestyles. [Hahnemann], [Vithoulkas]
Micro-comparison: Nux-v. has dyspepsia from excess with a driven, hot temperament; Cholinum is more “sluggish-metabolic,” with dullness and heaviness rather than spasmodic irritability. [Kent], [Clinical] Puls. has fat intolerance with changeable symptoms; Cholinum is less changeable emotionally and more rhythm-dependent (sleep and meals). [Kent], [Clinical] Remedy action is suggested when fatty food is tolerated better, nausea lessens, and the mind becomes less dependent on constant snacking to remain clear. [Clinical], [Vithoulkas]
Abdomen
Abdominal symptoms often resemble a hepatic-biliary congestion: right-sided heaviness, a dragging sensation, and a dull ache or tightness after rich meals, sometimes easing when lying on the right side (a clinical observation that can be confirmatory). [Clinical], [Hughes] Gas and distension may accompany mental strain and irregular eating, reinforcing the link between lifestyle rhythm and abdominal comfort. [Clinical] The abdomen feels better from warmth and gentle pressure, suggesting a sluggish, non-inflammatory pattern. [Boger], [Clinical] Stool colour may be described as lighter during sluggish phases, though this must be interpreted prudently and not over-valued without clinical context. [Clinical]
Micro-comparison: Chelidonium has strong liver and gall-bladder correspondence with scapular pains and marked right-sidedness; Cholinum may mimic the heaviness but is distinguished by the central cognitive fog, meal-skipping collapse, and sleep-linked crashes. [Clarke], [Hughes] Improvement is indicated when the abdomen feels lighter, digestion is steadier, and the patient’s mental clarity no longer fluctuates violently with dietary indiscretions. [Clinical], [Vithoulkas]
Urinary
Urinary symptoms are usually secondary. [Clinical] Some patients report increased frequency when anxious and depleted, and reduced output when congested and sluggish; these changes often track diet, sleep, and stress rather than local pathology. [Clinical] A faint fishy odour to perspiration or bodily secretions, when present, may be a confirmatory toxicologic echo (to be interpreted cautiously), especially if it appears with digestive upset and sweating. [Toxicology] Any pain, fever, blood, or acute urinary distress requires appropriate evaluation; the homeopath must remain responsible and individualise. [Hahnemann], [Vithoulkas]
Rectum
Rectal function often reflects the cholinergic-motility theme. [Clinical] Constipation may arise from sluggish peristalsis: stools are delayed, the urge is weak, and the bowel feels “lazy,” especially when the patient is fatigued or sedentary. [Clinical] In contrast, episodes of looseness may occur during dietary indiscretion or autonomic swings, with nausea and sweating, echoing the toxicologic direction without claiming a proving. [Toxicology], [Clinical] The key is variability tied to rhythm: when meals and sleep are regular, bowel function steadies; when they are chaotic, the bowel becomes unreliable. [Clinical], [Vithoulkas]
Micro-comparison: Alum. constipation is dry, inert, and obstinate with marked dryness; Cholinum constipation is more functional and rhythm-dependent, improving when the general state (sleep and nutrition) improves. [Kent], [Clinical] Remedy action is suggested when the bowel becomes regular without forcing, and the digestive heaviness reduces together with the mental fog. [Clinical], [Vithoulkas]
Male
In men, Cholinum may present as mental fog and reduced cognitive stamina with digestive heaviness, often worsened by irregular meals, alcohol, and sleep loss. [Clinical] Libido may be diminished chiefly from exhaustion and metabolic sluggishness rather than primary endocrine pathology. [Clinical] Irritability can arise from depletion: the man becomes short-tempered when hungry or tired, then improves after food and rest, a practical and characteristic pattern. [Clinical] The case must still be individualised; the remedy is not chosen because “choline is involved,” but because the modalities and generals repeatedly confirm. [Hahnemann], [Kent]
Female
In women, Cholinum may be seen in states of cognitive fog with pronounced dependence on meal rhythm and sleep quality, and a tendency to feel heavy and sluggish after fats. [Clinical] Emotional lability may be fatigue-driven: tears or irritability from depletion rather than deep grief. [Clinical] Some women notice worse fog and constipation with stress and irregular eating, and better clarity after a nap and a proper meal; this rhythm-dependence is central. [Clinical], [Vithoulkas] Again, prescribing must remain individualised, with careful follow-up in global function. [Hahnemann], [Vithoulkas]
Respiratory
Breath-holding while concentrating and sighing afterwards is common in overstrained states, worsening head fog. [Clinical] Gentle pacing and fresh air help; this aligns with the amelioration from open air and the need to remove obstacles to cure. [Hahnemann], [Vithoulkas]
Heart
Palpitations may appear with stimulant use, sleep deprivation, and hunger states; they are usually concomitants of autonomic instability rather than primary cardiac disease. [Clinical] Improvement is suggested when palpitations lessen as the patient’s rhythm (sleep, meals, reduced stimulants) and nervous stability improve. [Clinical], [Vithoulkas]
Chest
Chest symptoms are commonly secondary: tightness from stress, shallow breathing during concentration, and occasional palpitations when the patient is depleted, hungry, or over-caffeinated. [Clinical] These often improve in fresh air and quiet and worsen in heated rooms, repeating the general modalities. [Boger], [Kent]
Back
Dull hepatic region discomfort may be felt in the right mid-back or under the scapula as a heaviness after fatty meals, though typically less dramatic than classic biliary remedies. [Clinical], [Hughes] Neck tension accompanies mental effort and improves after rest and sleep. [Clinical]
Extremities
Extremities often show fatigue and heaviness: limbs feel “slow,” coordination is poorer when hungry or sleep-deprived, and mild trembling can appear after stimulants. [Clinical] Better after food, warmth, and rest; worse after irregular meals and late nights, which echoes the central modalities. [Clinical], [Vithoulkas]
Skin
Skin symptoms are secondary yet may include clammy perspiration during nausea episodes and stress-sweating. [Clinical] Occasional odour changes may appear as a toxicologic echo and should be weighed cautiously. [Toxicology]
Sleep
Sleep is a strong confirming field in Cholinum states. The patient often sleeps but does not recover: they wake with a heavy head and mental fog, as if sleep has failed to restore the nervous system. [Clinical], [Kent] Sleep deprivation is a major aggravation: one late night can worsen digestion, attention, and emotional steadiness, which ties directly to the “worse from lack of sleep” modality. [Kent], [Vithoulkas] There may be a late-afternoon crash followed by paradoxical evening wakefulness, where the person is exhausted yet restless, often after stimulants or heavy food. [Clinical] Naps can be remarkably restorative, producing a clear improvement in cognition and mood, which is one of the most practical confirmatory signs (better from sleep). [Kent], [Clinical]
Restless sleep may be accompanied by digestive discomfort: heaviness, nausea, or abdominal fullness, especially after rich evening meals; the patient then wakes unrefreshed and foggy. [Clinical] Sleep is often improved by a simpler evening routine: earlier light meals, fewer stimulants, and reduced stimulation; in Hahnemann’s language, these are obstacles to cure that must be removed. [Hahnemann], [Vithoulkas] Micro-comparison: Kali-phos. is prominent in nervous exhaustion with sleeplessness; Cholinum is suspected when sleep and cognition are strongly tied to meal rhythm and hepatic heaviness after fats. [Boger], [Clinical] Remedy action is indicated when sleep becomes truly restorative, morning clarity improves, and the patient’s cognitive stamina rises without constant reliance on snacking or stimulants. [Clinical], [Vithoulkas]
Dreams
Dreams may be dull, heavy, or food-related, with themes of eating, searching for food, or missing meals, especially in those whose symptoms are strongly hunger-linked. [Clinical] Alternatively, dreams may be anxious and disorganised during sleep-deprived periods, reflecting nervous overstimulation. [Clinical] Improvement is suggested when dreams calm and waking is clearer and steadier. [Clinical], [Vithoulkas]
Chill / Heat / Sweat
Cholinum states often show a sluggish chilliness and heaviness that is better in warmth, while oppressive heat and close rooms worsen fog and irritability. [Boger], [Kent] Sweating may appear during nausea or after dietary indiscretion as an autonomic discharge, reflecting a toxicologic echo. [Toxicology], [Hughes]
Food & Drinks
Food and drink are central to the Cholinum picture. Irregular meals aggravate: missed breakfast can bring fog, irritability, faintness, and poor concentration, while eating restores stability quickly. [Clinical], [Boger] Rich fats aggravate heaviness and nausea, especially late; the next day may be foggier, linking diet to sleep quality. [Clinical], [Hughes] Coffee and stimulants can produce a temporary push followed by a crash, worsening sleep and making the following day worse; this is a major maintaining cause in many modern cases. [Hahnemann], [Vithoulkas] Alcohol often worsens sleep and mental clarity and aggravates digestive heaviness. [Clinical] Improvement is seen when the patient naturally prefers regular, simple nourishment and becomes less “held hostage” by hunger swings and dietary indiscretions. [Clinical], [Vithoulkas]
Generalities
The Cholinum patient often feels metabolically slowed, as if the body and mind both move through thick mud: heaviness, fog, sluggish digestion, constipation tendencies, and low cognitive stamina. [Clinical], [Boger] The generals are strongly rhythm-based: worse from mental exertion, worse from sleep loss, worse from irregular meals and fasting, worse from rich greasy foods, worse in close heated rooms; better from sleep, quiet, fresh air, warmth, and regular meals. [Kent], [Boger] The patient frequently displays a threshold pattern: they can cope until hunger or fatigue crosses a line, then cognition collapses and irritability rises; after food and rest, they return to baseline. [Clinical], [Vithoulkas]
This remedy should be suspected only when the hepatic-biliary heaviness and the cognitive fog are part of one coherent picture with clear modalities, not when the case is better explained by classic polycrests. [Hahnemann], [Kent] Micro-comparison: Chelidonium is strongly hepatic with right-sided pain and marked biliary keynotes; Cholinum is more “nutrient-metabolic,” with cognition and rhythm dependence central. [Clarke], [Hughes] Another comparison: Nux-v. is overstimulated, irritable, driven; Cholinum is depleted, slowed, and rhythm-dependent, often improved more by nourishment and sleep than by purgation of excess. [Kent], [Clinical] Cure is recognised by broad improvement: steadier digestion, more consistent bowel rhythm, improved sleep restoration, and a clearer, more resilient mind. [Hahnemann], [Vithoulkas]
Differential Diagnosis
Aetiology and maintaining causes (overwork, sleep debt, stimulants, irregular meals)
- Kali-phos. – Nervous exhaustion with irritability and weakness; Cholinum shows stronger meal-rhythm dependence and fatty-food heaviness. [Boger], [Clinical]
- Nux-v. – Overdriven, irritable, stimulants, dietary excess; Cholinum is more sluggish-metabolic with fog that improves from regular nourishment. [Kent], [Clinical]
- Pic-ac. – Profound mental fatigue and prostration; Cholinum adds hepatic heaviness after fats and hunger-linked crash patterns. [Boger], [Clinical]
Liver-bile and fat intolerance themes
- Chelidonium – Strong right-sided liver-gall picture with scapular correspondence; Cholinum is more cognitive-metabolic and rhythm-based. [Clarke], [Hughes]
- Puls. – Fat intolerance with changeability; Cholinum is less changeable and more tied to fatigue/hunger cycles. [Kent], [Clinical]
Brain fog and confusion
- Anac. – Confusion with loss of confidence and mental conflict; Cholinum is more depletion-and-digestion linked. [Kent], [Clinical]
- Alum. – Slowness with constipation and dryness; Cholinum is more functional/rhythm dependent, less obstinately dry. [Kent], [Clinical]
Autonomic / nausea / sweat elements
- Tabac. – Nausea with cold sweat and collapse; Cholinum is typically less violent, more sluggish and meal-linked. [Clarke], [Kent]
- Cocculus – Nausea and weakness with motion; Cholinum nausea is more dietary/heaviness linked with fog. [Kent], [Clinical]
Remedy Relationships
- Complementary: Kali-phos. – When nervous exhaustion dominates, Kali-phos. may complement; Cholinum fits when meal rhythm and fatty-food heaviness are central. [Boger], [Clinical]
- Complementary: Chelidonium – When hepatic heaviness is strong, Chel. may lead; Cholinum may follow in the lingering metabolic-cognitive fog state. [Clarke], [Hughes]
- Follows well: Nux-v. – After the acute overstimulation phase is treated, Cholinum may suit the depleted “sluggish aftermath” with hunger crashes. [Kent], [Clinical]
- Related: Pic-ac. – Both cover mental fatigue; Cholinum is more digestive and rhythm-based. [Boger], [Clinical]
- Related: Alum. – Shared slowness and constipation tendency; differentiate by dryness/obstinacy vs rhythm dependence. [Kent], [Clinical]
- Antidotes (practical): late-night stimulants and heavy fats – Removing these obstacles clarifies action and restores sleep and digestion. [Hahnemann], [Vithoulkas]
- Inimical: routine prescribing by “nutrient theory” – Avoid prescribing because “choline is for the brain”; require characteristic modalities and generals. [Hahnemann], [Kent]
- Precedes well: convalescent support measures – Regular meals, sleep restoration, and pacing help the remedy act by removing maintaining causes. [Hahnemann], [Vithoulkas]
Clinical Tips
Cholinum is best considered when the case is dominated by brain fog + digestive heaviness + rhythm dependence: worse from fasting/irregular meals, worse from fatty foods, worse from sleep debt, better from regular nourishment and restorative sleep, with a dull, sluggish, heavy constitutional feel. [Clinical], [Boger] Because it is a modern substance without a deep classical proving, prescribe with caution, insist on strong confirmatory modalities, and judge success by broad functional improvement (clarity, stamina, digestion, sleep, bowel rhythm). [Hahnemann], [Vithoulkas]
Practical case management is often essential: stabilise meals, reduce late-night stimulants, lighten evening fats, and protect sleep; these remove obstacles to cure and allow remedy action to declare itself. [Hahnemann], [Vithoulkas]
Clinical pearls (brief):
- Foggy, irritable, and weak when breakfast is missed; markedly better after food and a short nap, with accompanying fatty-food heaviness. [Clinical]
- Dull hepatic heaviness and nausea after greasy evening meals, followed by unrefreshing sleep and morning brain fog. [Clinical], [Hughes]
- “Push-crash” cycle driven by coffee and irregular eating; improvement follows rhythm restoration alongside the remedy. [Clinical], [Vithoulkas]
Selected Repertory Rubrics
Mind
- Mind; concentration difficult; mental exertion; agg. – Core rubric for the cognitive collapse after study. [Kent]
- Mind; confusion; after mental exertion – Fog that follows thinking rather than preceding it. [Kent]
- Mind; memory; weakness – Especially functional, fatigue- and meal-linked forgetfulness. [Kent]
- Mind; irritability; from hunger – Irritability as depletion signal, not fixed temperament. [Clinical]
- Mind; sensitive; noise; agg. – Sensory gating failure during fog states. [Kent]
- Mind; desire; solitude; quiet – Relief by withdrawing from stimulation. [Kent]
Head
- Head; heaviness; from mental exertion – The loaded head after thinking. [Kent]
- Head; pain; after eating; rich food – Hepatic-digestive headache correspondence. [Clinical], [Hughes]
- Head; confusion; with headache – When fog and pressure travel together. [Kent]
- Head; vertigo; from fasting – Light-headedness from missed meals. [Clinical]
- Head; worse; close room – Stale-air aggravation is confirmatory. [Boger], [Kent]
- Head; better; open air – Fresh air clears heaviness and fog. [Boger], [Kent]
Eyes
- Eyes; complaints; from using eyes – Reading/screen effort worsens fog and headache. [Kent]
- Eyes; blurred vision; from fatigue – Processing fatigue rather than local disease. [Clinical]
- Eyes; aggravation; bright light – Sensory overload worsens the whole state. [Kent]
- Eyes; better; closing eyes – Relief by reducing input. [Kent]
- Eyes; weakness; evening – Coincides with the late-day crash. [Clinical]
- Eyes; complaints; from screens – Modern maintaining cause; valuable clinically when consistent. [Clinical]
Ears
- Ears; sensitiveness; noise – Noise penetrates and exhausts the mind. [Kent]
- Ears; noises; aggravate; headache – Auditory input worsening head pressure. [Kent]
- Ears; tinnitus; from nervousness – Often sleep- and stress-linked. [Kent]
- Ears; cannot endure many voices – Crowd noise as a trigger of confusion. [Clinical], [Kent]
- Ears; better; quiet – Silence as an immediate relief. [Kent]
- Ears; aggravation; close rooms – Stuffy environments worsen sensory intolerance. [Boger], [Clinical]
Stomach
- Stomach; nausea; after fatty food – A key hepatic-digestive pointer. [Hughes], [Clinical]
- Stomach; fullness; after eating; rich food – Heavy digestion and “stuck” stomach. [Clinical]
- Stomach; desire; food; frequent; small – Need to prevent hunger crashes. [Clinical]
- Stomach; worse; fasting – Weakness and fog from missed meals. [Clinical]
- Stomach; aggravation; coffee – Push-crash pattern; worsens sleep and fog. [Clinical], [Hahnemann]
- Stomach; better; after eating – Food restores stability and clarity. [Clinical]
Rectum
- Rectum; constipation; sluggish – Weak urge, delayed stool, functional inertia. [Clinical]
- Rectum; diarrhoea; after dietary indiscretion – Looseness as autonomic-digestive swing. [Clinical]
- Rectum; irregular stool; from irregular meals – Rhythm-dependent bowel unreliability. [Clinical]
- Rectum; constipation; from sedentary life – Overwork and immobility maintaining cause. [Clinical]
- Rectum; urging; ineffectual; from fatigue – Weak peristaltic drive in depleted states. [Clinical]
- Rectum; stool; better with routine – Regularity improves with stable rhythm. [Clinical], [Vithoulkas]
Sleep
- Sleep; unrefreshing – Sleep fails to restore clarity and stamina. [Kent]
- Sleep; worse; after heavy supper – Hepatic-digestive sleep disturbance pointer. [Clinical], [Hughes]
- Sleep; aggravation; from stimulants – Coffee/alcohol worsen sleep quality and next-day fog. [Clinical], [Hahnemann]
- Sleep; better; after a nap – Naps markedly restore cognition. [Kent], [Clinical]
- Sleep; waking; with head heavy – Morning fog with loaded head. [Clinical]
- Dreams; of food; eating; searching – Rhythm/hunger-linked dream content in some cases. [Clinical]
Generalities
- Generalities; weakness; from fasting – A key general when consistent. [Clinical]
- Generalities; worse; rich food; fats – Heaviness and sluggishness after fats. [Clinical], [Hughes]
- Generalities; worse; loss of sleep – Sleep debt aggravates the whole case. [Kent], [Vithoulkas]
- Generalities; worse; close rooms – Stale-air aggravation confirms. [Boger], [Kent]
- Generalities; better; open air – Clears fog and heaviness. [Boger], [Kent]
- Generalities; better; warmth – Sluggish chilliness and abdominal discomfort improve. [Boger], [Clinical]
References
Hahnemann — Organon of Medicine (1842): principles of individualisation, modalities, obstacles to cure, follow-up.
Hughes — A Manual of Pharmacodynamics (late 19th century): toxicologic reasoning and physiological correspondence in materia medica interpretation.
Kent — Lectures on Homeopathic Materia Medica (1905): valuation of generals, modalities, and nervous exhaustion states.
Kent — Repertory of the Homeopathic Materia Medica (1897): rubric framework and language.
Boger — Synoptic Key of the Materia Medica (1931): emphasis on modalities and clinical generals.
Clarke — Dictionary of Practical Materia Medica (1900): clinical comparisons, hepatic remedy differentiation method.
Phatak — Materia Medica of Homoeopathic Medicines (1977): differential reasoning and concise clinical pointers.
Boericke — Pocket Manual of Homeopathic Materia Medica (early 20th century editions): general prescribing principles and comparative style.
Vithoulkas — The Science of Homeopathy (1980): remedy reaction assessment, repetition cautions, obstacles to cure.
Sankaran — writings on miasms (1990s–2000s): miasmatic colouring as interpretive framework in chronic states.
Teixeira — methodology writings on modern provings/triturations (modern): standards for constructing reliable remedy pictures from contemporary substances.
Jansen — clinical writings on neurotransmitter and modern physiological remedies (modern): thematic clinical application and differentiation approach for modern substances.
Disclaimer
Educational use only. This page does not provide medical advice or diagnosis. If you have urgent symptoms or a medical emergency, seek professional medical care immediately.